What are the elements of quality control process in pharmaceuticals
- Kazi
- Last modified: April 2, 2024
Why do you need to implement a quality control process if you can manufacture products that are free from all possible contaminants?
Can you create a system that can eliminate all defects from a product? If possible, this can eliminate the necessity of quality control processes entirely. Until then, we must rely on quality control processes as part of quality assurance systems.
The risk of compromised patient safety for pharmaceutical products outweighs the risk of having no quality control process.
One of the main objectives of quality control is to test for product attributes that are known and expected. These attributes are part of the product specification.
However, laboratory testing cannot pick up all product defects if your test is not validated to detect unknown abnormalities. Your test may need to be more sensitive or may not be required for that product.
Companies, therefore, have to rely upon GMP rules and quality management systems to prevent these problems from occurring in the first place.
Why do you need to set up quality control process?
Quality control is the part of quality assurance systems that checks the quality of a batch after it has been manufactured. Quality control verifies that ingredients and products meet written and approved standards, often called “specifications.”
The quality control laboratory tests raw materials and finished product samples, which are randomly collected but represent the whole batch.
It is critical to get accurate results from quality control tests. Otherwise, defective batches may be released, and good batches may be rejected.
The role of the quality control laboratory is to detect any possible defects once they have occurred rather than to prevent them from occurring in the first place.
The quality control laboratory’s specific responsibilities include:
– Sampling, inspecting, and testing of starting materials and finished product
– Calculating and checking results against specifications
– Reporting all results and releasing on passed batches
Regulatory requirements for quality control process?
Quality control processes are regulated intensely by regulatory bodies for the right reasons. It is possibly the last processing gate to capture any defective products before they can be released into the market.
US FDA CFR 211 Sec. 211.160 General requirements state that,
(a) The establishment of any specifications, standards, sampling plans, test procedures, or other laboratory control mechanisms required by this subpart, including any change in such specifications, standards, sampling plans, test procedures, or other laboratory control mechanisms, shall be drafted by the appropriate organizational unit and reviewed and approved by the quality control unit.
(b) Laboratory controls shall include the establishment of scientifically sound and appropriate specifications, standards, sampling plans, and test procedures designed to assure that components, drug product containers, closures, in-process materials, labeling, and drug products conform to appropriate standards of identity, strength, quality, and purity.
Typical flow of samples in a quality control laboratory
The quality control laboratory receives samples that are collected randomly at the beginning, middle, and end of manufacturing processes. You should use a sampling plan based on the criticality of the defects and the size of the batch.
Some companies establish 100% in-line testing to generate additional assurance of quality.
After collecting the samples, they should follow a typical pathway inside the quality control laboratory, from receiving, testing, and preparing the final report.
Typically, laboratory samples follow sequentially, as shown below.
i. Receipt of samples in the laboratory
All laboratories maintain a sample-receiving register. This register logs the batch and sample number, the number of samples provided, and the time and date the sample first entered the laboratory. This is the commencement of sample tracking.
ii. Prepare samples and set up instruments
Many test methods require sample preparation before the test is run. The test method should describe exactly how the sample is prepared. This may involve simple dilution or more complex extraction and manipulation. Always refer to the current test method before setting up the sample.
iii. Run the test sample
Once the sample is prepared, it is included in the test run. Care must be taken to ensure that the sample is not degraded, e.g., by spillage, exposure to the atmosphere, or temperature degradation on the bench.
Always refer to the current test method for instructions on how to protect the sample during testing. While testing the sample, analysts should ensure that the instrument or a logbook records the sample number and it is traced exactly to the test result.
iv. Verify system suitability (if applicable)
For instrumental test runs such as high-performance liquid chromatography (HPLC) / gas chromatography (GC), the test method usually includes a verification that the entire instrumental system is performing satisfactorily on the day of the run.
This is called “system suitability testing” (SST). Non-instrumental methods may also include control or equivalent verification systems. The test methods should describe how the integrity of particular test runs is verified.
v. Collect raw data and calculate results
Once the sample has been run, either the instrument or the analyst will perform a calculation to arrive at a result. It is essential to double-check all calculations before finalizing sample results.
vi. How to deal with out-of-specification (OOS) results?
All quality control laboratories have written procedures for handling and investigating only results that appear to be out-of-specification. The analyst should ensure that the supervisor is notified as soon as an OOS event occurs, the sample is retained, and a documented investigation is commenced.
vii. Report the final result
Once the sample has been run, either the instrument or the analyst will perform a calculation to arrive at a result. It is essential to double-check all calculations before finalizing sample results.
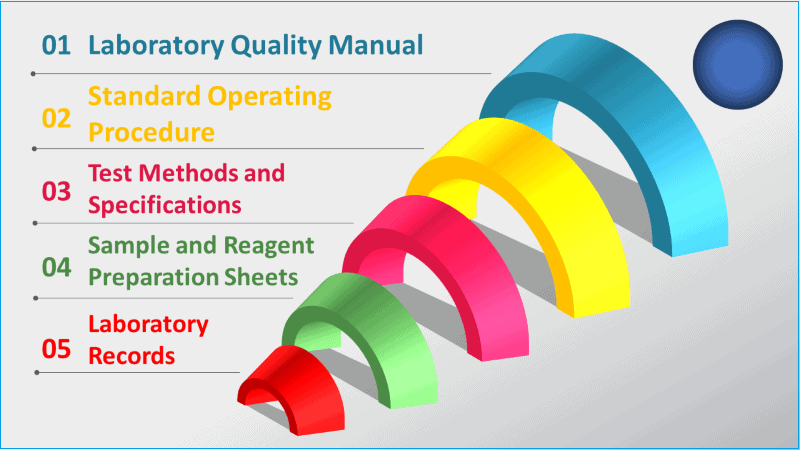
Essential elements of a quality control process
Quality control processes are complex, objective-oriented, and interdependent. It is a combination of a few essential elements, each complementing the other. Deficiency in one element directly impacts the overall effectiveness of the process.
The following are some common elements that are required to establish a good quality control process or system.
i. Laboratory quality manual and policies
Laboratory quality manuals and policies sit at the top of the quality control process hierarchy.
The quality manual should specifically describe or refer to:
– The laboratory quality policy, commitment, and objectives.
– The standard of service and governing standards (e.g., GMP).
– Laboratory SOPs and technical methods.
– How independence of judgment is demonstrated.
– The responsibilities and authority of key personnel.
– Qualifications and job descriptions (organizational structure).
– The management elements of governing standards.
– Deployment of the procedures, standards, and training for personnel.
– Quality assurance program (audit, review & improvement).
– Document control records management and archiving systems.
240 SOPs, 197 GMP Manuals, 64 Templates, 30 Training modules, 167 Forms. Additional documents included each month. All written and updated by GMP experts. Checkout sample previews. Access to exclusive content for an affordable fee.
ii. Quality control standard operating procedures
After establishing the laboratory manual, you must develop standard operating procedures as part of the quality control documentation system to remain consistent in your activities within the quality control.
Written procedures should reflect the requirements of governing standards. There are some essential procedures that are needed in almost all quality control processes.
– Laboratory management and organization
– Records, documentation, and archiving
– Reagent and standard quality control
– Test method validation and control
– Instrument calibration and maintenance programs
– Material and product specifications
– Quality, integrity, and authenticity of data
– Sampling procedures
– Personnel training
– Trend analysis, audits, and reviews, etc.
iii. Validated test method
A test method comprehensively describes all procedures used in sample analysis.
Analytical test method validation guarantees that your test method is robust enough to provide evidence if your product meets the predetermined product specification or conforms to the failure of a product.
Test method validation is the process by which it is established that the performance characteristics of the test method, such as precision, accuracy, specificity, linearity, limit of detection (LOD), limit of quantitation (LOQ), and robustness, meet the requirements for the intended applications.
Before commencing any assay, the analyst should refer to the current version of the test method. The test method should be available at the worksite.
vi. Qualified instruments
The quality control laboratory must process samples through qualified and calibrated instruments. The analyst should be aware of the status of the instrument before conducting the test.
In particular, the analyst should pay attention to the instrument calibration status. Do not proceed with the test if an instrument is out of calibration.
Upon introduction to the laboratory, all laboratory instruments should undergo formal qualification.
v. Reference standard
Many tests require comparison of the sample to an official reference standard.
Reference standards can be either primary or secondary (sometimes called working standards).
The primary standards are authentic materials with very high purity. The pharmacopeias and regulatory agencies recognize primary standards as the official industry standards for particular tests.
Secondary reference standards are also substances of established quality and purity, usually prepared in-house. The same core should be taken in preparing the secondary reference standard as is taken when preparing the sample for the test.
The analyst should ensure that only the current and approved reference standards are used for testing. The reference standard number must be recorded in the test record.
vi. Approved specification
All quality control laboratories must have a set of published and approved specifications for each starting material and finished product.
When calculating and checking results, the analyst should refer to the current specification to decide the status of the sample. These specifications are often registered with the regulatory agency and cannot be changed.
vii. Employee training
Employee training is an essential requirement under good laboratory practice (GLP). Laboratory personnel must be trained before they are approved to perform the job. Untrained personnel will eventually make errors and mistakes that can compromise product quality.
It is a GMP rule that staff are trained on the approved documents applicable to their work areas and must sign to the effect that they understand the requirements.
viii. Internal GMP audits
Internal GMP audits or self-inspections are requirements under good laboratory practice (GLP). The purpose of an internal audit is to independently check that the rules and documents established by the quality assurance team are being followed.
Internal GMP audits also provide opportunities to improve procedures and practices in the factory.
ix. Dealing with out-of-specification results
Laboratory result out-of-specification events are a common occurrence in the quality control process. A laboratory investigation is required before any repeat assays are conducted if a single assay result does not meet the agreed specification.
The laboratory must determine, if possible, whether a laboratory error, sample, or batch failure is the cause of the out-of-specification result.
The Investigation should be documented according to a written procedure.
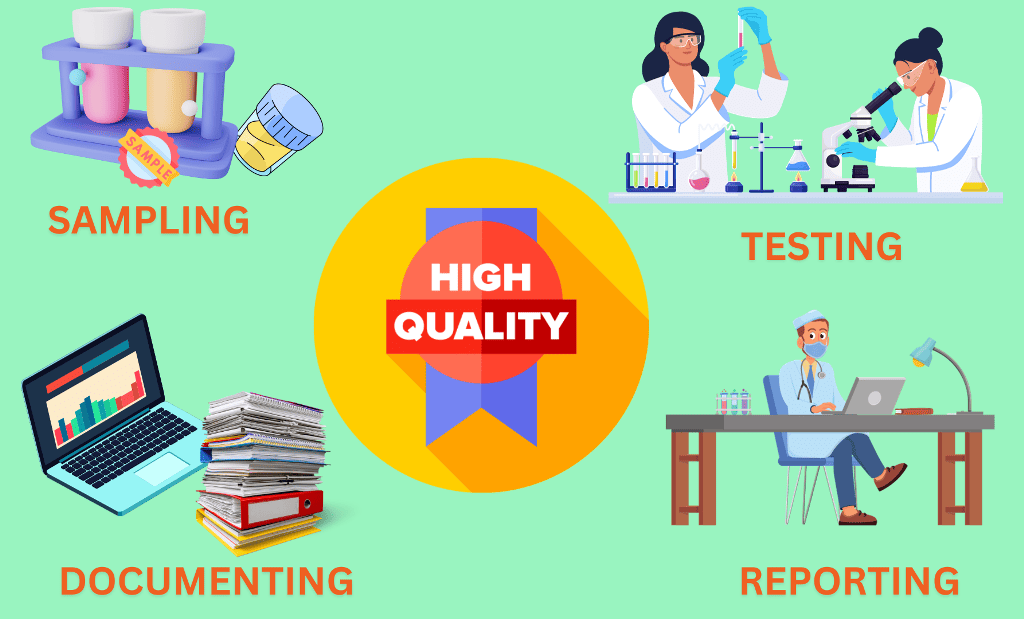
Common activities performed in quality control laboratory
Quality control compliance encompasses many activities documented in the GMP rules. These activities are common across different industries like pharmaceuticals, food processing, and medical devices.
i. Sampling of materials
The sampling of starting materials and finished products is completely governed by GMP regulations. You must document all sampling procedures and plans in use.
If wrong or insufficient samples are taken, or a poor sampling technique is used, any subsequent testing may then give misleading results.
As a result, a good product may be rejected, or, much worse, a defective product may be released.
ii. Testing of laboratory samples
Testing of samples in the laboratory is a mandatory requirement under GMP regulations. Its effectiveness, though, is limited because the entire batch cannot be tested, nor can the batch be tested for all types of potential contamination.
In fact, quality control testing is limited to looking for defects after they have occurred, so it is not a QA prevention system but rather a defect detection system.
iii. Maintaining laboratory records and documentation
Each product has a specific set of specifications registered with the government authorities. Starting materials and finished products are required to be tested to these specifications, and the results are reported to quality assurance if there is a problem.
Batches may not be released to the market if results do not conform to the approved specifications.
iv. Complying with GLP requirements
GMP rules that are applied to the quality control laboratory are sometimes called G(Control)LP rules, or G(C)LP. These G(C)LP rules are also checked during laboratory audits:
– Conduct tests to approved, written test methods.
– Calibrate and quality instruments.
– All samples and standards are traceable and accounted for.
– Complete test records accurately and in real-time.
– Validated methods support all tests.
– Record or capture all generated raw data directly, promptly, and legibly.
– Use traceable data sheets or sequentially numbered notebooks.
– Date and sign or initial data entries on the day of entry.
– Archive records so that they are protected, secured, and easily retrievable.
Typical documentation in a quality control process?
The laboratory documentation is designed to ensure there is linkage between the standard procedures and test methods (what is required to do?) and the laboratory records (what was actually done?).
This forms the laboratory records quality system.
240 SOPs, 197 GMP Manuals, 64 Templates, 30 Training modules, 167 Forms. Additional documents included each month. All written and updated by GMP experts. Checkout sample previews. Access to exclusive content for an affordable fee.
ii. Laboratory quality manual
The laboratory quality manual and laboratory policies are top-level documents describing the overall management and organization of the laboratory. These documents should reflect the requirements under GMP rules.
When you develop laboratory quality policies, consider including the following Items in your policies.
– Conflict of interest, ethics, and reference standards.
– Maintained and deployed procedures for laboratory operations and tests based on referenced methods for testing.
– Sample handling to maintain the integrity of the analytical data.
– Maintenance of records to facilitate retrieval.
– Employment of qualified and trained personnel.
– Routine maintenance of laboratory data to support test results.
– Maintenance of an instrument calibration program that provides measurement traceability to the international system of units (e.g., SI units).
– Change control for management systems and test methods.
ii. Standard operating procedures
Standard operating procedures (SOPs) provide more detailed and specific requirements for each laboratory quality element.
For example, SOPs describe how to handle a sample, conduct an audit, release a result from the laboratory, and manage a complaint. SOPs are generally not specific to test methods.
Following are some common key SOPs for quality control Laboratories. QC staff should be familiar with the following key SOPs:
– Management structure, responsibility, and authority
– Apparatus and instrument use and maintenance procedures [per instrument)
– Record keeping, reporting, storage, archiving retrieval systems
– Completion of laboratory records, workbooks, logs, and registers
– Handling out-of-specification (OOS) conditions
– Release of results from the laboratory
– Sample receipt identification, labeling, handling, traceability, and protection
– Analytical method validation and change/updates
– Computer security restrictions and data entry
– Reference standards control
– Laboratory calibration and performance check program
– Retention samples control
– Training programs
iii. Test methods and specifications
Test methods provide specific stepwise directions on how to properly execute a test procedure in a standardized manner.
A test method is specific to analysis and for instrumental techniques such as HPLC. Specifications generally accompany test methods and provide pass/fail criteria and acceptance criteria for a test method, such as system suitability or control limits.
iv. Sample and reagent preparation sheet
Sample and reagent preparation sheets are used to document the instructions for preparing laboratory solutions, standards, and working reagents.
It is important in a laboratory to provide accurate instructions and records of these preparations.
Usually, these sheets are linked to specific test methods. Equally important are the instructions for calibrating standard solutions.
v. Laboratory records
Testing records include quality control laboratory analyst notebooks, specific testing sheets, analytical printouts, electronic records such as chromatographs, and ancillary records that support the laboratory’s compliance.
Ancillary records would include calibration reports, training records, and monitoring of the environment.
vi. Specifications
Specifications are documented for starting materials, in-process products, and finished products. These specifications are submitted to the regulatory authorities when products are first registered.
If specifications need to be altered for whatever reason, approval must be sought from the government regulators.
The finished product is required to meet the specifications throughout the full shelf life under the approved storage condition.
vii. Altering records in quality control
A critical part of the quality control process is ensuring the reliability of results.
One way to ensure that the results are error-free is to conduct a second check of calculations and raw data. This check should be independent, that is, done by a different analyst or supervisor.
The following activities should be double-checked:
– The record has been completed to quality control standards.
– Current approved test methods and specifications were used.
– There was an accurate recording or summary of results from the chromatographs.
– All calculations are accurate.
– Replicate results are internally consistent.
– There were no deviations from the approved test method.
– Results reported are within specification.
Observations, data, and calculations shall be recorded when they are made and identifiable to the specific task.
When mistakes occur in records, each mistake shall be crossed out, not erased, made illegible, or deleted, and the correct value entered alongside.
All such alterations to records shall be signed or Initialled by the person making the correction. In the case of records stored electronically, equivalent measures shall be taken to avoid loss or change of original data.
Types of specifications in a quality control process?
Each batch must conform to the respective specification when tested. All out-of-specification (OOS) conditions must be investigated.
Pharmacopoeias are legal standards for the quality of products and materials. They specify the quality attributes of products and materials in “monographs” and provide information on how tests should be conducted.
i. Starting materials specification
In the pharmaceutical industry, the requirements for starting materials must be well-defined and documented to ensure that you get the material specified or ordered and that there are no mix-ups.
Starting materials are defined by a standard name, the supplier’s/ manufacturer’s code, and a unique item code.
Specifications for starting materials should include:
– Inspections and/or tests required
– Reference to test methods and acceptance criteria
– Material storage conditions
– A retest or expiry date
– Reference to pharmacopeial method (if available)
– Approved supplier and manufacturer (if available)
– Sampling instruction or reference
– Any precautions
ii. Intermediate product specifications
In the pharmaceutical industry, specifications for intermediate and bulk products should be available if these are received or dispatched or if data obtained from tests on intermediate or bulk products are used for the evaluation of the finished product or further processing.
The specifications should be similar to specifications for starting materials or for finished products, as appropriate.
iii. Packaging material specifications
In the pharmaceutical industry, the requirements for pre-printed packaging materials must be well-defined and documented to ensure that you get the items you specified or ordered and that there are no mix-ups.
A standard name and a unique item code define packaging materials.
You should include the following items in the packaging materials specifications:
– A detailed description of the item
– Inspections and/or tests required
– Acceptance criteria
– An approved label copy
– Approved supplier and manufacturer (if available)
– Sampling instruction or reference
– Storage conditions
– Any precautions
vi. Finished product specifications
You should include the following items in the finished product specifications:
– An exact statement of the active material
– The product code (if any)
– The dosage form and/or strength
– Physical appearance and identity
– All tests and their limits
– Details of, or reference to, the test methods
– Sampling instructions
– The shelf life and storage conditions
– Designated name
– Package details
– Formula (or reference to a formula) any precautions
240 SOPs, 197 GMP Manuals, 64 Templates, 30 Training modules, 167 Forms. Additional documents included each month. All written and updated by GMP experts. Checkout sample previews. Access to exclusive content for an affordable fee.
Test method validation in the quality control laboratory
The quality control laboratory is required to demonstrate that all test methods are reliable. This means they must be validated by verifying the following attributes:
– Precision (amount of variation in the assay)
– Accuracy (difference between the average results and the “true” value)
– Selectivity (ability of the method to measure the analyte in the presence of interfering compounds)
– Sensitivity (limit of quantitation or limit of detection of the method)
– Linearity and range (over what range the method measures the analyte in direct proportion)
– Ruggedness (how the test method Is affected by reasonable changes)
If a test method is not validated, it is difficult to be assured that the results are reliable.
GMP requires that all critical steps of manufacture are reliable or validated. This naturally includes laboratory test methods.
How to perform sampling in quality control process
Sampling is the removal of a presentative portion of a lot to understand the lot’s composition and characteristics.
Pharmaceutical sampling procedures are carried out during and at each major processing step during manufacturing to ensure the highest quality is attained.
The purpose of testing samples is to make some inference about the lot from which the sample is drawn:
– To determine the quality level
– To detect a certain level of defects
– To assess the level of heterogeneity
– To identify mix-ups, mislabelling, or contamination
It is assumed or accepted when sampling that:
– There is an agreed or implied inherent risk in any conclusions.
– Defects are randomly distributed in the batch.
– The production process is stable and continuous.
i. Sampling limitations
No matter how well or how often QC testing is conducted, there is always some risk that defects are not detected in the lot.
This means that a defective product could be released even though it passed all the tests. If one wanted to be 100% sure that a batch does not contain any defects, every unit of the batch would have to be tested. Since this is not practical, you have to accept some risks.
Despite these limitations, GMP regulations require companies to conduct quality control tests routinely. However, when you properly follow GMP regulations during manufacture and packaging, it will help prevent defects from occurring in the first place, which reduces the company’s reliance on quality control testing.
ii. Sampling plan and risks
Sampling plans decide which lots of products to accept and release, and which lots to reject and either rework or discard.
Ideally, a sampling plan should reject all “bad” lots while accepting all “good” lots. However, because the sampling plan bases its decision on a sample of the lot and not the entire lot, there Is always a chance of making an Incorrect decision.
This is termed the sampling risk. If a good lot is rejected incorrectly, this is called the supplier’s risk. Conversely, if a poor lot Is accepted Incorrectly, this is called the consumer’s risk. Sampling plans generally try to set these risks between 5% and 10%.
Naturally, the way the sample is selected has a big impact on the level of risk.
What is corrective and preventive action (CAPA) in quality control?
A corrective action is an action to eliminate the cause of a detected nonconformity, and a preventive action is an action to eliminate the cause of a potential nonconformity.
Corrective actions are required to eliminate the causes of an existing nonconformity, defect, or other undesirable situation. Corrective actions are taken to fix a defect on hand.
On the other hand, preventive actions are implemented to prevent potential non-conformances in the future. Preventive action is taken to fix the cause of a problem before it can happen. The future risk mitigation measures are clear examples of preventive action.
Neither the FDA CFR 211 regulations nor international GMP standards specifically mandate CAPA systems as part of the quality assurance system. However, they are implied and expected. ICH Q10 makes this requirement more explicit.
i. Requirements for corrective actions
Your organization must take action to eliminate the cause of nonconformities in order to prevent recurrence. Corrective actions should be appropriate to the effects of the nonconformities encountered.
According to ISO 13485, you should prepare a documented procedure to define corrective action requirements for:
– Reviewing nonconformities (including customer complaints),
– Determining the causes of nonconformities,
– Evaluating the need for action to ensure that nonconformities do not recur,
– Determining and implementing action needed,
– Records of the results of any investigation and of the action taken
– Reviewing corrective action taken and its effectiveness.
ii. Requirements for preventive actions
You should determine action to eliminate the causes of potential nonconformities in order to prevent their occurrence. Preventive actions should be appropriate to the effects of the potential problems.
As per ISO 13485, you should establish a documented procedure to define requirements for preventive actions.
– Determining potential nonconformities and their causes,
– Evaluating the need for action to prevent the occurrence of nonconformities,
– Determining and implementing action needed,
– Records of the results of any investigations and of action taken and
– Reviewing preventive action taken and its effectiveness.
iii. CAPA Register
The register provides a list of CAPA events and their current status. From the register, Supervisors can tell which CAPA events are the most common and what stage they are at in being resolved. The register will also be of interest to government auditors.
The best practice of CAP management should have the following features:
– In built risk assessment
– A means to trend CAPA to identify related issues
– Assigned responsibilities for CAPA actions
– A system for identifying when a CAPA closeout has not been met
– Integration with management review meetings
iv. CAPA phases
The CAPA system can be broken down into four distinct phases, each of which requires different actions, different outcomes, and probably different responsibilities.
For a detailed explanation you can check the article Six Step Procedure for corrective and preventive action.
240 SOPs, 197 GMP Manuals, 64 Templates, 30 Training modules, 167 Forms. Additional documents included each month. All written and updated by GMP experts. Checkout sample previews. Access to exclusive content for an affordable fee.
a. Initiating CAPA event
A potential CAPA can be initiated from multiple different sources or events:
– External events or marketplace feedback such as complaints, adverse events, or service reports.
– Manufacturing nonconformities such as errors, process deviations, laboratory out-of-specifications, or starting material failures.
– Quality management system noncompliance originating from, for example, documented procedures, internal audits, regulatory audits, or product or process trend reviews.
– Poor product design
CAPAs can also originate from opportunities to improve any of the above.
b. Raising the CAPA
Not all problems or issues necessarily warrant a CAPA report. Companies should put in place business rules that qualify an issue as a CAPA.
One of the key tools for qualifying for a CAPA is risk assessment. Generally, applying risk assessment to an issue will answer the question: “Does this incident merit a further investigation and a CAPA?”
If a CAPA is raised, it should be formally documented using a CAPA form and assigned a unique tracking number. Responsibility is then assigned for conducting an investigation and root cause analysis. There are no particular rules regarding who should assume responsibility, but often, it is the group or person that knows most about the problem or will derive benefit from its resolution.
c. The CAPA plan
This phase is about ensuring that there is a clear CAPA action plan based on the investigation and root cause analysis in the previous phase.
The plan should be approved, actions to be taken should be set out, responsibilities assigned, and target completion or progress review dates nominated for particularly large CAPAs, a formal project plan would be useful.
The CAPA plan should be approved by the quality representative and the area management before implementation. The plan should also be linked to change controls where they apply.
d. Implement, monitor, and close
The last phase of a CAPA is to implement the approved plan and track its progress against agreed dates.
Once a CAPA plan is implemented, it is necessary to verify that it has been effective by monitoring the Impact of the actions. The verification could be immediate or delayed until the CAPA impact becomes evident. It is usual to keep the CAPA in “open” status during the monitoring phase until it is formally closed.
Conclusion
Since no one can create a system that can eliminate all unknown defects from a product, we must rely on quality control process to guarantee product quality and safety.
The main objective of quality control is to check the quality of a batch as it was manufactured. The ideal ways of implanting quality control tests are at the starting, middle, and end of the manufacturing process. Sometimes, you have to implement 100% quality control checks, especially in those circumstances where the manufacturing process isn’t stable, or the product is too sensitive to environmental factors.
Quality control processes are complex. To guarantee the operational success of a quality control laboratory, you have to create high-level manuals and policies, standard operating procedures, validated test methods, use qualified instruments, and train your analysts at a minimum.
You have to build a process to check the test results against predetermined parameters, also called specifications. There are specifications for starting materials, packaging materials, intermediate, and finished products.
If, at any time, the laboratory test results fall outside of those specifications, you should investigate the incident as out-of-specification, identify the root cause, and implement corrective and preventive actions.
There are strict rules and requirements from the regulatory authorities on how the quality control processes should be established. Generally, they are called Good Laboratory Practices. You must always ensure that you are complying with those requirements through periodic audits.
Quality is everyone’s responsibility, and it should pervade every aspect of pharmaceutical manufacture and packaging. Quality should not be tested into products; instead, it must be built in at each step of manufacture.
Quality manifests itself not only in obvious ways, such as during actual processing steps, but also in diverse areas, such as vendor assurance, personnel training, internal audits, change management, release for supply, and QC sampling.
Pharmaceutical manufacturers must integrate the key functions of the quality control process. The primary objective of this is to check for defects as they have occurred.
240 SOPs, 197 GMP Manuals, 64 Templates, 30 Training modules, 167 Forms. Additional documents included each month. All written and updated by GMP experts. Checkout sample previews. Access to exclusive content for an affordable fee.

Author: Kazi Hasan
Kazi is a seasoned pharmaceutical industry professional with over 20 years of experience specializing in production operations, quality management, and process validation.
Kazi has worked with several global pharmaceutical companies to streamline production processes, ensure product quality, and validate operations complying with international regulatory standards and best practices.
Kazi holds several pharmaceutical industry certifications including post-graduate degrees in Engineering Management and Business Administration.